Preservation Of Fertility
Preservation of fertility means the application of medical, surgical and laboratory procedures to preserve the potential of conception with the individual own eggs or sperm in adults and children at risk of sterility during reproductive years.
Individuals at risk for decreased fertility include:
- Women, men and children exposed to chemotherapy, radiation and surgery for cancer treatment.
- Individuals receiving chemotherapy and radiation prior to bone marrow transplantation e.g relapse in Hodgkin or non-Hodgkin lymphoma, leukemias, sickle cell anemia.
- Individuals exposed to chemotherapy for non-cancer conditions e.g lupus nephritis and other connective tissue disorders
- Individuals requiring removal of gonads e.g removal of both ovaries to reduce cancer risk in women susceptible to breast-ovarian cancer syndromes, BRCA genes and removal of ovarian cysts.
- Individuals with chromosomal abnormalities that are associated with premature loss of eggs e.g some patients with Turner syndrome.
Without intervention, these conditions are expected to reduce the potential for conceiving genetic children by 50% or more compared to unexposed individuals according to The Childhood Cancer Survivor Study in the US and The Norwegian Radium Hospital study in Scandinavia.
The risk of loss of fertility potential should be promptly evaluated prior to treatment by a reproductive endocrinologist with special expertise in the methods of preservation of fertility. Women inquiring about fertility potential after cancer treatment were more likely to be referred for consultation to a fertility specialist.
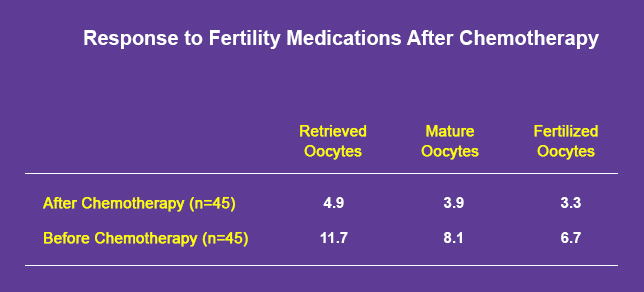
Resumption of cyclic menstrual function and even normal blood work (e.g FSH) does not accurately reflect damage to reproductive organs due to cancer treatment. We have shown that even in women with normal cycles after exposure to chemotherapy and normal FSH levels, response to fertility medication and subsequently the number of eggs obtained is markedly reduced, hence the need for preservation of oocytes, sperm or embyos before disease treatment. Antimullerian hormone (AMH) appears to be a better indicator for ovarian reserve after exposure to chemotherapy.
Preserving Fertility In Women : Ovarian Stimulation In Estrogen Sensitive Cancer
Estrogen sensitive tumors include breast cancer, cancer of the uterus, thyroid cancer, melanoma and possibly some cancers affecting the brain and the ovary. Breast cancer represents more than ¼ of tumors affecting women. The use of fertility medication is associated with marked increase in estrogen levels. To prevent this rise a special method for ovarian stimulation Dr. Azim has investigated the use of a special medication to prevent the rise in estrogen during stimulation. After intermediate follow up (about 2 years) there was no apparent increase in the risk of breast cancer recurrence using this method. The article was published in the Journal of Clinical Oncology in 2008.
Embryo Cryopreservation
Stimulation of the ovaries, retrieving the eggs and fertilizing them with sperm and freezing the resulting embryos is the standard and most successful method for preservation of fertility. Cancer in itself does not appear to affect the response to fertility medication but cancer treatments do. Thus it is important to consider a plan for fertility preservation prior to starting cancer treatment to enhance the outcome of preservation of fertility.
Oocyte Cryopreservation
Freezing of oocytes is an option for preservation of fertility in women with no current partner (and do not prefer to use a sperm donor). Oocyte vitrification yields a better outcome than slow freezing of eggs as explained in section on egg freezing.
Ovarian Tissue Freezing
This is an experimental method for preservation of fertility. It is usually employed when treatment carries a very high risk for ovarian failure, when there is no time to stimulate the ovaries to freeze embryos / oocytes or in children.
The ovary is removed using laparoscopy (outpatient surgery), cut into thin slices and frozen for later use. After cancer treatment is concluded, the slices are thawed and transplanted. There have been six babies born worldwide using this method after transplanting the tissue back into the abdominal cavity.
Preserving Fertility In Men
Sperm Cryopreservation
The most successful and simplest approach. One or multiple sperm samples are obtained and frozen. Sperm can be later thawed and used for insemination or IVF.
Testicular Tissue Freezing
Pieces of the testes can be frozen for later use. Transplantation of testicular tissue is still an investigational technique.
To help organizing your understanding of your fertility potential after cancer diagnosis and to co-ordinate care with multiple providers, consider the checklist below:
Who To Ask : Oncologist
Questions
- Type of cancer
- Stage
- Treatment Plan
- Surgery
- Chemotherapy
- Bone marrow transplant
- Radiotherapy
- Hormonal treatment
- Is Preservation of fertility suitable for me?
- Ask for a referral letter.
- Obtain medical records:
- surgery records
- pathology records
- Other tests: ER, PR, her2/neu, BRCA
- general medical tests
Who To Ask : Reproductive Endocrinologist
Questions
- How is cancer and cancer treatment expected to impact my future fertility?
- What are the suitable options for preservation of fertility?
- Embryo freezing
- Oocyte freezing
- Ovarian tissue banking
- Others
- Combination
- Is it safe?
- What to do with the frozen embryos, eggs or tissue after cure?
- What is the success rate for my options?
- Blood work: FSH, estradiol, AMH
- Ultrasound
- Semen analysis
- Other general tests required for IVF and cell and tissue freezing
- Co-ordinate fertility preservation plan with the oncologist
Who To Ask : Support groups
Questions
- Help with referral
- Help with medications
- fertilehope.org
- youngsurvival.org
- lbbc.org
