In Vitro Fertilization (IVF-ICSI)
During an IVF cycle, the ovaries are stimulated with hormonal medications, eggs are retrieved and fertilized. The resulting embryos are grown in an outside media for an average of five to six days. At this stage the patient has the option to freeze the embryos or proceed with a fresh embryo transfer.
In vitro fertilization can be an emotional and financial commitment. We may postpone this treatment plan until we have considered other treatment paths, though in some cases, IVF may be the only option for a patient experiencing severe male and/or female factor infertility.
IVF Entails Stimulation Of The Ovary To Produce More Than One Oocyte (Preferably 5-10).
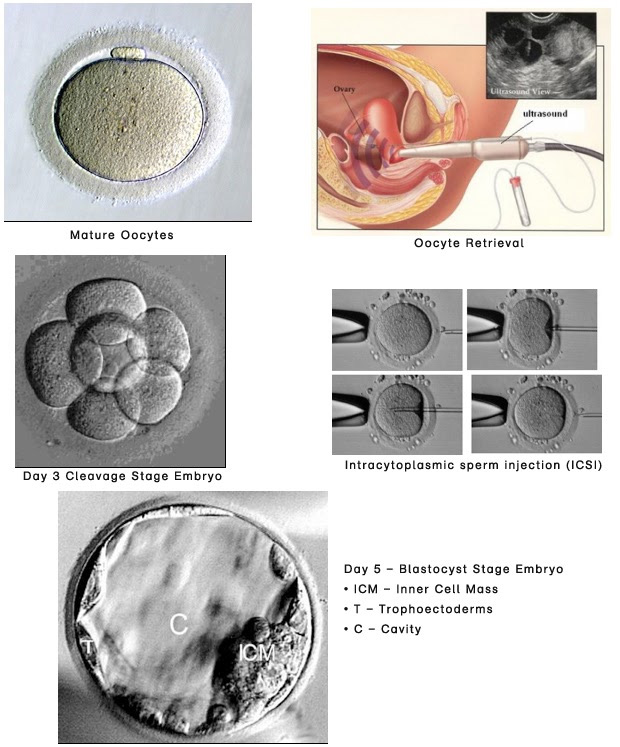
Oocytes are harvested by a simple outpatient procedure through the vagina, fertilized by sperm in the lab. Resulting embryos after fertilization are observed in a culture dish for 3 to 6 days. Fertilization takes place by surrounding the mature oocyte with 50,000 sperm or by directly injecting one sperm into the egg (ICSI). One or more embryos are then selected for transfer into the cavity of the uterus. The second half of the cycle (luteal phase) is then supplemented by progesterone (vaginal or injection). Female partner is tested for pregnancy about 2 weeks later. Surplus embryos are frozen for later use.
Ovarian Stimulation
A synthetic hormone (FSH) very similar to the one produced by the master gland in the brain is used to stimulate the ovary to produce more than one egg. This is usually combined with another medicine (agonist or antagonist) to prevent the master gland from triggering ovulation prematurely, before the eggs are mature and ready for fertilization. When the follicles are judged to be mature based on their size and estrogen levels, ovulation is triggered using an injection (hCG; human chorionic gonadotropin or agonist).
Finesse in using the appropriate starting and maintenance dose and timing the trigger injection is crucial to successful outcome (adequate number of mature oocytes) and minimizing complications (ovarian hyperstimulation syndrome-OHSS).
Women are classified according to their response to ovarian stimulation (based on age, ovarian reserve blood tests and number of antral follicles) into high responders and low responders.
High Responders
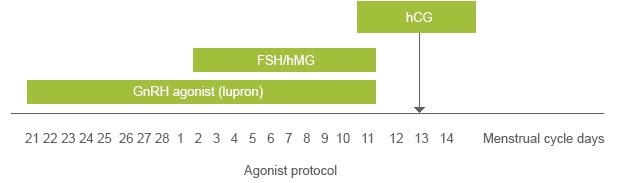
The aim of ovarian stimulation is the production of moderate number of mature oocytes (around 8 to 10) while avoiding ovarian hyperstimulation syndrome. Lower dose of FSH is used with frequent monitoring of ovarian response to modify the dose if needed. The use of gonadotropin releasing hormone antagonist has the added advantage of using an agonist instead of hCG for the final trigger shot. Unlike hCG, the agonist does not over-stimulate the ovary and is not associated with OHSS. Low stimulation reduces the potential harmful effects of high FSH on oocytes and those of very high estrogen on the lining of the uterus. It also reduces the cost of ovarian stimulation.
Low Responders
The aim is to improve ovarian response by modifying multiple aspects of ovarian physiology including synchronization of follicles prior to the onset of stimulation. A modified natural cycle approach entails avoiding stimulating medications and observation of natural follicular growth. When the follicles reach an advanced stage, follicular growth is supported by a very low dose of FSH. Another approach used in low responders entails using estrogen and antagonist prior to starting ovarian stimulation to synchronize the follicles prior to stimulation and increase the oocyte yield.
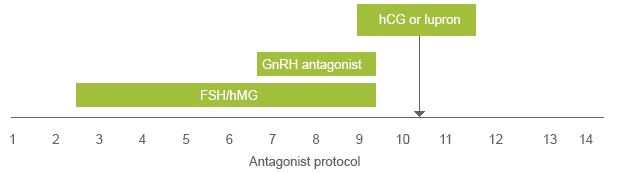
Other methods also include increase in production of women’s own internal hormones (FSH) from the master gland using clomid or flare lupron.
ICSI/IMSI
In Intracytoplasmic Sperm Injection (ICSI), sperm is injected into the egg in the lab. This method is used when the quantity/quality of sperm is low such that the sperm is unable to fertilize the egg. Currently this is the most advanced technology in IVF treatment. This is recommended for severe male factor infertility or prior poor fertilization results.
Intracytoplasmic morphologically selected sperm injection, or IMSI is a specialized technique for ICSI where a high magnification digital imaging lens is used to select the best sperm for injection into the egg. This highly sophisticated technology is preferable in cases of abnormal sperm morphology (shape) or previously failed ICSI to improve fertilization outcomes.
Safety
Achieving high pregnancy rates after fertility treatment is a priority. It is equally important, however, to accomplish this goal in the safest possible way. The two most prominent risks of fertility treatment are ovarian hyperstimulation syndrome (OHSS) and multiple pregnancies Severe OHSS occurs as a result of excessive exposure to fertility medication (FSH) followed by exposure to hCG. It is more common in younger women and women diagnosed with PCOS. The syndrome is characterized by excessive bloating, vomiting, diarrhea, ascites (fluid accumulation in the abdomen), increased concentration of blood constituents and blood clotting. We are successful in avoiding the syndrome in most cases through careful selection of initial and maintenance dose of FSH, stopping FSH for few days (coasting), using an agonist (lupron) to trigger final oocyte maturation (instead of hCG) and sometimes cancelling embryo transfer and freezing all embryos (to be used later in a thaw cycle). There is no firm evidence that IVF and its related procedures directly increase the risk for any cancer or birth defects in children.Multiple pregnancies (twins or more) are associated with higher risk of preterm delivery, need for intensive care admission for the babies and sometimes long term health problems. Mothers carrying multiple babies are at increased risk for anemia, hypertensive disease in pregnancy, postpartum hemorrhage and cesarean delivery. Careful determination of the number of embryos to be transferred can minimize the risk for multiple pregnancy.
Extended Embryo Culture And Blastocyst Transfer
Embryos are usually placed in an incubator for 3 days after egg retrieval before transferring them to the uterus. Extending the culture to day 5 or 6 (blastocyst stage) allows for better selection of embryos that may have a higher implantation potential. This approach is favored in women with 4 or more embryos when the plan is to transfer 1 to 2 embryos.
Embryo Transfer
This is a procedure that requires a lot of thoughtful planning. The aim here is to introduce the embryos into the middle of the cavity of the uterus without damage to them or the uterine lining and without exciting uterine contractions. The cervix is inspected to determine its shape and direction. Ultrasound also delineates the cervical canal. Trial transfer is performed prior to the actual procedure to detect any difficulties. Difficulty in embryo transfer can reduce the chances for pregnancy.
The actual procedure is monitored with abdominal ultrasound so that the direction of the cervical canal is visualized and accurate placement of the catheter tip is ensured.
Sometimes, the cervix requires dilatation prior to transfer or the transfer can be done through the wall of the uterus avoiding the cervical canal (trans-myometrial embryo transfer).
